
| Vol. 14 No. 1 | Summer 2004 |


by Phil Sahm
Thanks
to a powerful new MRI scanner, U of U doctors and researchers can better
help those suffering from multiple sclerosis, autism, cardiovascular
disease, and more.
To live with multiple sclerosis (MS) is to live with uncertainty.
An inflammation of the brain and spinal cord that disrupts communication between nerve fibers, MS strikes no two people in exactly the same way. Some it debilitates, taking away the motor skills needed to speak, walk, or perform other everyday tasks; others it treats less severely, allowing them, in varying degrees, to continue with their lives. Everyone who has MS harbors the fear that it will eventually rob them of their ability to function at all.
 |
|
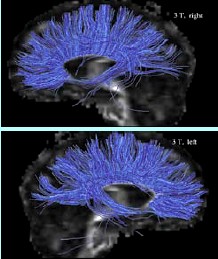
Using
diffusion tensor imaging — and the 3T’s powerful resolution
— autism researchers can look more closely at the fibers that
allow different parts of the brain to communicate. |
The cause of MS is unknown, and tracking its course has been tricky for neurologists, the physicians who specialize in diseases of the brain. The best tool they have is magnetic resonance imaging (MRI), a way to take pictures inside the body to see disease, organs, bones, and tissue. When the first MRI scan was performed in the late 1970s, it marked a giant technological leap from X-rays, but it’s only been in the past few years that MRI scans have become powerful enough to show subtle details that may signal change or progression in disease.
Last summer, the University Health Sciences Center took a step toward raising the bar on MS research when the foundation of longtime benefactors Ian and Annette BS’68 MBA’83 Cumming donated one of the most sophisticated and powerful MRI scanners in the world to the U of U. If one picture is worth a thousand words, the $3 million Magnetom 3T Trio System MRI is an encyclopedia at the fingertips of U neurologists, radiologists, other physicians, and researchers. With the 3T’s powerful images of the brain, neurologists can see MS more clearly than ever, enabling them to give patients the best treatment available.
The Cummings donated the 3T in honor of David G. Bragg, M.D., former chair of radiology at the U School of Medicine, and J. Richard Baringer, M.D., professor and former chair of neurology. But their donation had a personal meaning, as well: their son John was diagnosed with MS more than four years ago.
 |
| Autism researchers William M. McMahon, M.D., and Janet E. Lainhart, M.D. |
MRI is a way of using magnets, radio waves, and computers to make images of the inside of the body. Made by Siemens Medical Solutions, the 3T magnet is twice as powerful as most MRI scanners and provides superior images of spinal abnormalities, the brain, tumors, cardiovascular disease, and more. For example, doctors can view a 3T image and know whether a patient’s heart wall is getting enough blood, how well the heart is pumping, and if the coronary artery is blocked. Housed at the U of U’s Center for Advanced Medical Technologies in Research Park, the 3T can reveal whether a tumor is recurring or responding to treatment, and, in some cases, even whether it’s benign or cancerous. Problems with joints, cartilage, and degenerative diseases are easier to identify, and the 3T sees minute changes in brain biochemistry—which opens vast possibilities for studying MS.
The scanner’s impact on clinical care, research, and teaching at the University will be huge, according to E.A. “Steve” Stevens, M.D., professor and chair of radiology at the medical school. “We are going to see and understand the human body better than we ever have,” Stevens says.
The new MRI was barely up and running before John W. Rose, professor of neurology, was taking scans of his MS patients. Aside from being a little noisier, a 3T scan isn’t much different from other MRIs. But the results provide the clearest and most detailed pictures of MS that Rose and his patients have seen. MS shows up as spots, or lesions, in the white matter of the brain, and the 3T’s detailed images help Rose tell how, or if, a patient’s disease is progressing. In many cases that allows him to offer something that MS patients have seldom received in the past—reassurance that their MS is not getting worse.
John Cumming, who is also one of Rose’s patients and was diagnosed with MS in his early 30s, quips that his first 3T scans immediately brought good news: “I still have a brain.” Images showed areas of his brain where he and Rose knew there were MS lesions, but the powerful 3T images also showed spots they didn’t know MS had affected. The scans showed many more details of the damage to his optic nerve and upper spinal cord, and these new pictures prompted Rose and Cumming to make subtle changes in his medication and medical regimen.
Cumming hopes the 3T helps doctors and researchers learn
more about treating his MS, but he also hopes his role in MS research
will benefit others with this mysterious disease. “It’s a
pretty lonely walk to have MS,” he says. “I’m proud
to know I’m helping.”
Rose and other U researchers expect to advance MS research considerably
with the 3T’s help. Along with physicists Dennis L. Parker PhD’79,
professor of radiology, and Eun-Kee Jeong, research associate professor
of radiology, Rose and other researchers at the Utah Center for Advanced
Imagery Research are studying how to image the spinal cord of MS patients.
The role of the spinal cord in MS is an area that has received little
notice and is ripe for discovery, according to Rose.
“We are looking forward to applying the full technology of the 3T,” he says. “We’re going to raise the bar considerably.”
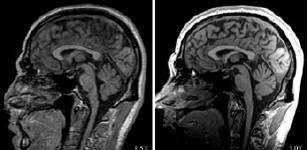 |
Then and now: Scan pictures of the same individual show the marked improvement in quality from the 3T scanner (right) vs. a 1.5 scanner (left). Images courtesy of Tracy Abildskov and Dr. Erin Bigler, Utah Autism Research Program. Images courtesy of Tracy Abildskov and Dr. Erin Bigler, Utah Autism Research Program. |
MS is still a long way from being cured or prevented. Right now, as with many diseases, it would be a victory to stop the disease from getting worse in those it strikes. Rose hopes the 3T may help with that by providing images that allow earlier diagnosis and show how well treatments are working. Eventually, he wants to use the 3T to develop a battery of tests to diagnose MS earlier.
While Rose and his colleagues research the enigma of MS, two U of U psychiatrists are taking advantage of the 3T to study another baffling neurologic ailment: autism. Autism is a disorder of early brain growth and function that impairs basic aspects of social, language, and communication development.
The School of Medicine is one of 10 major U.S. medical centers participating in a research network by the National Institute for Child and Human Development (NICHD). The NICHD has designated the U one of 10 “Collaborative Programs of Excellence in Autism” (CPEA) sites to investigate the disorder on three fronts: genetics, immunology, and brain development (neuroimaging). The U of U is the only CPEA in the Intermountain Region and one of only two inland sites between the East and West coasts, according to Janet E. Lainhart, M.D., associate professor of psychiatry and the study’s co-principal investigator.
William M. McMahon, M.D., associate professor of psychiatry, is the study’s principal investigator. Hilary Coon, research associate professor of psychiatry, is leading the genetics portion to gather genetic information from 800 Utah families that have at least one member with autism. Robert S. Fujinami BS’72, professor of neurology, is determining if immunological mechanisms are involved. The genetics and immunology data will be integrated with brain imaging for a full study of autism.
In the neuroimaging part of the study, U researchers are following 72 children and adults with autism, as well as a control group of 72 people without autism. The study will track the brain development of children with autism into adulthood to look for clues to understanding the disorder. Participants will receive an MRI scan and clinical neuropsychological assessment at the beginning of the study and another three years later. The 3T will be critical in helping U researchers track brain development in people with autistm over a period of years, according to Lainhart, who also heads the neuroimaging portion of the study.
“It is quite clear from our work to date, and the work of other investigators, that the key to the neurobiology of autism and brain mechanisms involved in autism lies not in how the brain looks at any one time,” Lainhart says. “Rather, the key lies in how the brain changes over time.”
The number of people with autism in the United States is unknown, but the disorder is estimated to occur in two to six people per thousand, according to the Centers for Disease Control and Prevention. This means the total could range from 580,000 to nearly 1.8 million Americans. Mental retardation is associated with the disorder, but autism occurs at all IQ levels, even into the 140s. One-third of children with autism do not speak, and the disorder can be difficult to diagnose before age 2.
Other than increased brain size in young children with autism, there are no major structural differences between the brains of people with autism and those who develop more typically. That fact leads researchers to suspect the brains of people with autism have other problems. The current thinking is that some areas of the brain are not communicating properly, according to Lainhart. “It’s like parts of the brain are normal in size and shape, but the wiring is just not right,” she says.
| If one picture is worth a thousand words, the $3 million Magnetom 3T Trio System MRI is an encyclopedia. |
With the aid of the 3T’s powerful resolution, the U researchers will track minuscule changes in brain development of people with autism. Sophisticated image analysis methods will demarcate the gray and white matter of the brain and map changes in the size and shape of brain regions over time. The 3T brain image data on children and adults will be combined, and then brain volume and gray and white matter will be statistically compared between autistic children and adults and those who are developing normally.
Employing diffusion tensor imaging, a technique that uses the dispersal of water molecules through cells, the researchers will look more closely at the white matter in the brains of study participants. Gray matter consists of neuron cells on the surface of the brain in the cortex and deep in the brain. These cell bodies send out white matter fibers, or axons, that connect different parts of the brain and allow them to communicate. Diffusion tensor imaging allows much more detailed study of white matter, including how fibers are organized.
“The exquisite quality of 3T images lets us look closer
and better at brain development in autism,” Lainhart says. “There
is no doubt we will learn much more about autism with the 3T scanner than
was possible in the past.”
As information is gathered, U of U researchers hope it will help them
put together a clearer picture of autism that may lead to therapies to
treat or even change the course of the disorder. “The time is ripe,”
says Lainhart. “Most researchers are optimistic and hopeful that
within the next 10 years, maybe five, we’ll have a much better understanding
of autism.”
Diffusion tensor imaging has potential applications for other disorders and diseases, such as strokes, MS, amyotrophic lateral sclerosis (Lou Gehrig’s disease), tumors, and spinal cord injuries.
 |
| The Mabey family hopes the 3T scanner will help U researchers learn more about 14-year-old Nick’s autism. |
Fourteen-year-old Nick Mabey might help reveal autism’s
mystery by taking part in the study.
Nick, who is considered “high functioning,” was 2½
years old when he was diagnosed with autism, after his parents had spent
a frustrating year trying to find out what made him bang his head against
the wall and repeatedly flick light switches on and off. But his parents
got him help, and today he would be considered lucky among those with
the disorder. He converses well and goes to a mainstream public school
in his town of West Bountiful, Utah, where he takes special-education
and mainstream classes. Nick excels in both French and mathematics, according
to his mother, and enjoys watching television—Pokémon—riding
his bike, and playing with his Game Boy. Like many people with autism,
though, Nick has a hard time with social skills and making friends. He
underwent his first 3T scan as part of the study in late February.
“They did it to see how the brain works and what causes
autism so they could somehow find the cure,” he says.
But Nick isn’t looking for a cure at the moment. Right now he has
his sights on a more immediate goal: the ninth-grader wants to go to Viewmont
High School next year—where his father went.
Whether the 3T helps University researchers learn enough about autism to help her son is yet to be seen, but Tammy Mabey, like the parents of other autistic children in the study, is taking the long view, happy her son is contributing to the research.
“If it doesn’t help Nick, maybe it will help others,” she says.
—Phil Sahm BS’78 is a writer in the Office
of Public Affairs for the U’s Health Sciences Center.