 |
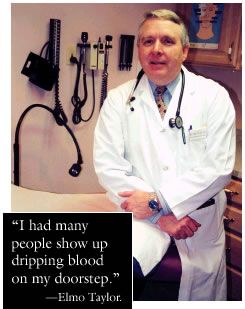
It’s 2 a.m. in Bicknell, Utah, and Elmo Taylor PA’78 hears someone knocking on his door.
Opening it, he finds a man
standing before him, slightly drunk, bleeding from his forehead. The man
claims that he has just been in a fight.
“He was too big to fit on my kitchen table,” remembers Taylor,
“so he laid down on my living room floor and I began suturing his
forehead.” With Taylor’s Labrador retriever keeping a watchful
eye on the patient—and the patient just as carefully eyeing the dog—Taylor
finished the procedure in the stillness of his sleeping house. The suturing
having had a sobering effect on the patient, Taylor was able to send him
on his way (and to learn later that the “fight” was actually
a rollover). “And sitting there with my dog, that was when I thought,
Well, I guess this is what rural medicine is all about,” Taylor recalls.
Almost 200 miles to the north, a man enters the Fourth Street Clinic in
Salt Lake City, yelling, “I need my TB medicine or I’m going
to die!”
The physician assistant on duty, Peter Chapa PA’95 MSPH’95,
discovers that the agitated patient had been under treatment for tuberculosis
in another city—and that, in addition to the TB medication, he needs
housing, treatment for alcoholism, and counseling. Quickly.
 Working
from a hierarchy of greatest needs, Chapa and others at the clinic coordinate
with social-service organizations to get the patient his TB medication,
a bed in a respite care facility, a space in an Alcoholics Anonymous program,
and, eventually, a spot in a state-administered Directly Observed Therapy
(DOT) program in a shelter.
Working
from a hierarchy of greatest needs, Chapa and others at the clinic coordinate
with social-service organizations to get the patient his TB medication,
a bed in a respite care facility, a space in an Alcoholics Anonymous program,
and, eventually, a spot in a state-administered Directly Observed Therapy
(DOT) program in a shelter.
Today, and several fortunate vacancies later, the patient works, keeps
his appointments, takes his medication—and, Chapa adds, “has
friends—people who care about him.” Chapa himself continues
to spend each day at the clinic seeing new faces, “each presenting
with unique challenges.”
When it comes to PAs—physician assistants—Chapa and Taylor,
graduates of the Utah Physician Assistant Program (UPAP) at the U, are,
well, a little unusual. Taylor was named national “Rural PA of the
Year” in 1989 and Chapa was named national “Inner-city PA of
the Year” in 2001. But what they do—quite well—is what
most PAs do. They are on the front lines of health care: the first and
sometimes only person that most patients encounter, the general practitioner
who sees every patient and every ailment, the point of entry to a sometimes
inhospitable health-care system.
“During the course of a day, I may see 20 to 30 patients, and every
one of them is different,” Taylor says. “I never know what’s
going to be behind that door when I open it.” Chapa agrees. “I
take patients one at a time,” he says, “and I always have to
be on my toes.”
Direct patient care is the cornerstone of the University’s PA program,
which is currently in its 30th year of operation. “Our basic premise
is ‘service to the underserved,’” says Don Pedersen PhD’88,
director of the program. “Seventy-five percent of our graduates are
in primary care, and 40 percent are in communities of 10,000 or less.”
And, he points out, most of those PAs stay in their practices for a long
time. “They don’t want to move into administrative ranks; they
feel they’ve really made a commitment to patients.”
PAs at the U complete an intensive two-year graduate program in the School
of Medicine. Like other PAs, they are licensed to practice medicine with
a supervising physician; they are, in Pedersen’s view, “an extension
of a doctor’s practice.” In most states, including Utah, they
can prescribe medicine.
Both Chapa and Taylor clearly
enjoy the one-on-one interaction with patients. Chapa, who had worked
as an emergency medical technician and a laboratory medical technician
prior to enrolling at the U, says, “I liked the medical part of being
a med tech, but I didn’t like being stuck in a lab all day.”
Even-tempered and nonjudgmental, Chapa is a crucial link for homeless
patients whose everyday world is far different from the institutional
world of health care.
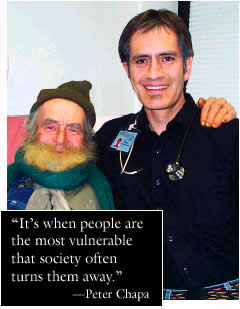 “I
started in homeless health care 12 years ago,” Chapa says. “I
knew I wanted to work with low-income people. It’s where there’s
the greatest need for, but the least access to, health care. Working with
the homeless was more challenging than I thought it would be at first.
These people are living on the streets, malnourished, often substance
abusers, and have psycho-social issues. So the health-care issues are
complicated by so many other issues.”
“I
started in homeless health care 12 years ago,” Chapa says. “I
knew I wanted to work with low-income people. It’s where there’s
the greatest need for, but the least access to, health care. Working with
the homeless was more challenging than I thought it would be at first.
These people are living on the streets, malnourished, often substance
abusers, and have psycho-social issues. So the health-care issues are
complicated by so many other issues.”
Observing Chapa’s waiting patients—tired looking and sometimes
bundled in several layers of clothing, wearing everything they have on
their backs—it’s clear that he is often their sole portal to
many needed services. To care for his patients, who see him for everything
from respiratory ailments and the flu to complications from diabetes,
hypertension, and liver disease, the seemingly unflappable Chapa has had
to construct a dual life. “When I first started, it was overwhelming.
But now I try not to be frustrated by the things I can’t do and by
the things the patients can’t comply with. When I go home, I try
to leave it all behind.”
Like Chapa, and like most who enroll in the PA program, Taylor had prior
health-care experience. “My first training was in the military. I
was an Army medic and did a tour in Vietnam,” he says. “It was
horrendous.” A member of the National Guard, Taylor is still a medical
officer for an artillery unit.
Today, Taylor practices at the Westside Medical Clinic in Clinton, Utah,
but for 11 years, he served the 2,000 people in Wayne County, Utah (including
the 350 people in Bicknell), taking care of “everything from emergency
childbirth to gunshot wounds.” (In fact, the first baby he delivered,
he says, “was a breech baby in the back of an ambulance.”) It’s
still the interaction with patients that draws him to his work. “The
most gratifying part of my job now is the continuity of care,” he
says. “I’ve seen people since they were little kids, and now
they bring their own kids in.” In fact, the affable Taylor says that
in Bicknell, he was almost too available to the community. “I had
a lot of sidewalk consultations, people stopping me at church or in the
grocery store to ask about a medical problem. I was essentially on call
24 hours a day, seven days a week”—not surprising, since his
supervising physician was in Richfield, 60 miles away, and visited Bicknell
only once a week.
The need for health care in rural communities was central to the creation
of the physician assistant program in Utah. With a shortage of primary-care
physicians in the late ’60s, C. Hilmon Castle, M.D., and William
Wilson created the Utah Physician Assistant Program and its precursor,
the Utah Medex Project.
Thirty years later, UPAP has graduated 700 PA practitioners; it’s
the only PA program in the state and one of only a few in the region.
Nationally, there are 129 accredited programs, and more than 40,000 people—including
Chapa and Taylor—were in clinical practice as PAs at the beginning
of 2001. A recent national report on PAs showed that solo physicians who
utilize PAs significantly increase the number of patients seen, decrease
patient waiting time, and spend more time with patients answering questions
and providing preventive care. It’s no wonder that “physician
assistant” is listed as one of the top 10 fastest-growing occupations,
according to the U.S. Department of Labor, with a projected growth of
48 percent from 1998 to 2008.
As front-line practitioners, PAs also grapple with one of the biggest
impediments to health-care access: money. Though both Chapa and Taylor
see improvements in the system—Chapa in the better facility in which
his clinic is housed and Taylor in the numbers of people being reached—they
both worry about the costs of basic ser-vices.
“We have the best health-care
system available,” Taylor points out, “but can we finance it?
Nowadays, with managed care, things are so insurance driven. If a company
changes its insurance carrier, then patients are displaced, and that can
be hard.” At the Fourth Street Clinic, where 95 percent of the services
are free to eligible patients, “we can only provide as many services
as are funded,” Chapa says. “Most of our funding comes from
federal grant money, and we get some state money, along with donations.”
Even meeting the most basic needs of the homeless patients—shelter,
food, and clothing—can be difficult if the social-service funding
isn’t available.
Witnessing Chapa and Taylor at work in their clinics is a reminder of
the importance of those fundamentals. For parents with a sick child, the
elderly suffering chronic pain, or the homeless who are habitually ignored,
interaction with a knowledgeable, caring human being surely expedites
recovery. As Chapa points out, “I think a little kindness goes a
long way.”
—Theresa Desmond is editor of Continuum.
