
VOL. 9 NO. 4 THE MAGAZINE OF THE UNIVERSITY OF UTAH SPRING 2000
Hope Finds A Home
by Adam OlsonHow, with a billionaire's help, the University of Utah built on genealogy and genetics to become a world leader in the race to cure cancer.
Lynn Trenbeath MA'81 is well acquainted with cancer. It has been a part of her family for a long time. Her grandmother died of breast cancer. Her mother's cousin died of breast cancer. Her mother had a lump removed from her breast five years ago.
So when doctors cut cancer from her own breast just six months after her mother's mastectomy, they weren't removing a stranger. It was an expected, albeit unwelcome, event.
Naturally, Trenbeath was concerned that her daughter, Erin Trenbeath-Murray BS'91 MS'94, would be next. Her oncologist, Dr. Saundra Buys, director of the High Risk Breast Cancer Clinic at the Huntsman Cancer Institute (HCI), encouraged Trenbeath to enroll in the clinic with her mother and daughter.

Part of the clinic's research is genetic testing for the mutated BRCA 1 and 2 genes that almost unavoidably lead to breast cancer. If the genes were found, Trenbeath-Murray could expect to follow in her mother's footsteps.
"The idea of getting cancer is pretty scary," says Trenbeath-Murray, who currently teaches at the University. "But I've been planning on it for several years."
 |
| Dr. Sandra Buys |
When her test results came back, they were negative. HCI doctors didn't find the mutated BRCA 1 or 2 genes. But rather than feeling excited, Trenbeath-Murray was apprehensive.
"When they didn't find the gene, I was disappointed," she says. "It was back to the unknown." But the clinic asked her and her family to stay. "We fit the pattern of inherited breast cancer," Trenbeath-Murray says. "So they wanted to continue studying us.
"There could easily be a BRCA 3 or 4 gene that they just haven't discovered yet," she adds. "Hopefully, with our participation, they'll find something before my own daughters are grown up." And though the fate of her family includes being plagued by cancer, Trenbeath-Murray also has the benefit of living in the vicinity of a billionaire chemical industry executive whose family shares the same plight.
When a Philanthropist Bankrolls Science
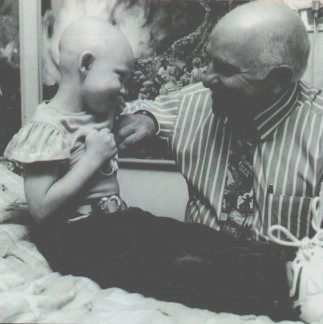
 Jon Huntsman Sr. |
Since the gene-mapping effort of the early 1980s, the University of Utah has been making progress toward becoming a world leader in human genetics. The Huntsman Cancer Institute, formed in 1995, is building its cancer research efforts on that genetic foundation.
"If you ask us about where we rank among cancer centers, you have to include a lot of well-established centers," says Raymond White, founding executive director of HCI. "We're not yet in that league, as we're still young and we don't have a dedicated cancer hospital. But we are really seen as world leaders in molecular approaches to human genetics. So if you ask us where we rank in the world as far as our human genetics and cancer genetics, we're at the top."
Last September, White relinquished his administrative duties to focus his full energies on leading new studies to understand the fundamental basis of cancer. Dr. Stephen Prescott, HCI senior research director, assumed the executive director's duties. In his new role, White is responsible for strategic scientific issues, including evaluation and incorporation of new technologies. In addition, he leads a joint venture with the California biotechnology firm Incyte, a project that seeks to identify new cancer-causing genes and new ways to treat cancer with fewer side effects.
The Huntsman Cancer Institute is composed of University faculty members for whom HCI is a second hat. Many of the researchers at HCI are from the University's Human Molecular Biology and Genetics program or the Department of Human Genetics. Both of the programs are housed in the Eccles Institute of Human Genetics. Unlike the Huntsman Cancer Institute, where "institute" refers to a group of people, the Eccles Institute is the building itself.
Now in its fifth year, HCI was created with a $100 million gift from Jon M. Huntsman Sr. Last fall members of the Huntsman Cancer Institute completed a move into their new $65 million, six-floor home east of University Hospital. The new center, with its stylish appointments, looks more like a corporate headquarters than a hospital, and is staffed with 300 researchers lured from the top laboratories in the nation. Huntsman calls it a refuge of hope.
Aside from the High Risk Breast Cancer Clinic, HCI began with four cancer programs: one each for prostate cancer, colon cancer, and brain cancer, and the Children's Cancer Specialty Clinic, operated jointly with neighboring Primary Children's Medical Center.
"We have a very interesting organization here at the Huntsman Cancer Institute," says Jon Huntsman Jr., president of the Huntsman Cancer Institute. "We looked at a couple of models in bringing this idea to fruition."
One of those models was the Howard Hughes Medical Institute—a national organization made up of researchers who belong to different schools and laboratories across the country. Researchers work in their own laboratories, and the Hughes Institute has various offices around the nation. It rents the fifth floor of the Eccles Institute of Human Genetics, which houses the laboratories of researchers Brenda Bass, Mario Capecchi, Dr. Mark Keating, Dr. Jean Marc Lalouel, Dr. Louis J. Ptacek, and Carl Thummel.
"The Howard Hughes organization didn't provide the flexibility that we were looking for," Huntsman says. "So we came up with this." HCI officials wanted to have a policy-setting oversight board—the Huntsman Cancer Foundation—that included Huntsman family members as well as University administrators.
HCI also has a four-member scientific advisory board—with two Nobel laureates—that meets with HCI investigators each year to determine whether the work being done in the laboratories is contributing sufficiently to major advances in cancer. "We have around this table the best minds for setting the agenda for research," says Huntsman Jr., "both from the basic academic standpoint and the practical 'how do you translate this into something that makes sense' standpoint."
As the senior Huntsman told the Associated Press, "I love the term entrepreneurial science. I know it makes scientists nervous because there's a sense of having to return a report. And that's great. That's why we give the money, so we can get results. We've got to have a bottom line." But how did the University get to where it is today—having a cancer research center that administrators feel will be one of the top cancer centers in the nation within a few years?
From Hut to Huntsman's Help
It has taken 150 years for the University to go from holding classes in a single-room adobe house to being a leader in genetic cancer research. But White says to understand what has allowed HCI to blossom, one must understand what makes HCI unique: the use of human genetic approaches. It was just two decades ago, in the early 1980s, that the University made its largest steps in genetics.
The system for mapping human genes that White developed while working in the Department of Human Genetics (of which he was the co-chair) led to the ability to identify the specific inherited genes that, when expressed, lead to a disease. There have been many applications for such a powerful tool. White pondered his own background and interests, and devoted himself to inherited cancer genes.
 |
| Raymond White |
"The general technology has been used by thousands of laboratories to map hundreds of genes, and identify hundreds of genes," White says. "We focus on cancer. Gene mapping was an enabling technology."
As the Department of Human Genetics grew, the Eccles Institute of Human Genetics was built with private funding from the Howard Hughes Medical Institute and the George and Dolores Doré Eccles Foundation. Upon completion of the building, a new effort, the Eccles Program for Human Molecular Biology and Genetics, was begun. Prescott was the founding director of the program. He served in that capacity until just before the dedication of the Huntsman Cancer Institute building.
The genetics programs at the University have continued to grow. From the 90 who started the Department of Human Genetics in 1984, there are now more than 750 people involved in that department, the Program for Human Molecular Biology and Genetics, and the Huntsman Cancer Institute.
But the University's strong human genetics programs are only a part of the story. The catalyst that made the Huntsman Cancer Institute a reality was the family for which it was named.
"I lost my mother to breast cancer in the 1960s, before she could ever really know any of her grandchildren," Jon Huntsman Sr. says. "Later, I lost my father to prostate cancer—four years after they said he was cured. I decided early on that if I could ever give $1 million, $500,000, $2 million—if I ever had the resources, if I was ever successful enough—I would give what I could to fight cancer."
Then, in the early 1990s, Huntsman himself battled prostate cancer.
"After being cured, I got the family together to decide what we could do. We decided that we should extend ourselves beyond anything we had ever done. The donation is essentially all our free revenue."
Committed to Going Out of Business
The Huntsmans know that their involvement in the Institute is not a one-time effort.
"We don't know exactly what will be needed next—whether it's in the research or clinical areas," says Huntsman. "But when the need arises, the family will have to decide what to do."
It hasn't taken long to decide. Work is already in the preliminary stages for a clinical facility or "cancer hospital" to the north of the new building. The newer facility's nature and scope are not fully defined but will include clinical programs, clinical research, and care.
"We want to add a high-quality clinical component," White says. "And with that, in 20 years I'd put [HCI] in the top 20 [cancer centers in the nation]."
Along with physical growth, the Institute is focusing on expanding the reach of its research. Prescott says that HCI is already developing programs for skin and ovarian cancers, and sarcomas. The Institute is currently investigating resources on campus in order to pull those programs together.
For the Huntsmans, the sooner they can move forward, the sooner they will reach their goal. "We'd like to go out of business ultimately," says Huntsman Jr. "We'd like to close down the institute or change the course of direction to some other human, genetically-based disease. It would mean that we had found something that has eradicated cancer as a disease."
"The goal of the Huntsman Cancer Institute is a very practical one," says Prescott. "It is to relieve the suffering of people with cancer."
But even with all of the advances made in recent years, how close are researchers to actually reaching that goal? "That's really impossible to answer," Prescott says. "I don't think any of us would give the same answer."
"I don't know how far off we are," says Dr. Joseph Simone, senior clinical director and director of the Huntsman Cancer Care Program. "We can cure some cancers in some people now. About 50 percent of cancer patients today are cured. The other 50 percent are much harder and will take longer. It depends on what stage of what cancer under what condition. Cancer is very complex. It is a bunch of different diseases at different stages of growth and development."
 |
|
Dr.
Joseph Simone
|
Adds Jon Huntsman Jr., "When you look at the complexity of cancer and see that there are 70 to 80 different types—each of which needs to be approached a little bit differently and uniquely—the totality of the job ahead strikes you. It is an ominous undertaking for these researchers.
"It's not going to be a magic bullet, by any stretch. It's going to be a disease-by-disease approach to discovering cures and therapies," he says.
One of the targets for HCI researchers is better understanding of the precursor stage of a number of cancers.
 |
| Dr. Stephen Prescott |
"Most cancers go through a transition," Prescott says, "from normal to abnormal—but not truly cancerous—to, frankly, a killer. Our greatest chance is if we find ways to diagnose cancers...in this precursor stage. At that intermediate stage they're much easier to treat and there's a much greater chance of completely abolishing them."
Prescott is optimistic that "as often as we can find the so-called precursors, we'll develop very good treatments for the cancers, whether medical or surgical."
"We think that intervention at the very earliest stages of cancer is the real hope for the future," says White. "As evidence that that's not unrealistic, reports show that intervention at the intermediate stage of colon cancer prevents 75-80 percent [of those cases from becoming cancer]. In the case of colon cancer, that intermediate stage is called the colon polyp. It probably exists 10 to 15 years before cancer emerges—and it's visible to the gastroenterologist. Not only can he see it, but he can clip it out.
"So starting in your early 50s, you see your local gastroenterologist every few years. If he clips out any polyps that he finds, it reduces your colon cancer risks by 75 to 80 percent. That's huge. This is a 50,000-deaths-per-year disease. That's 40,000 people who don't need to die," according to White.
On the Pathway to Discovery
The Huntsman Cancer Institute's approach to curing cancer is trying to find the stepping stones on what its leaders call the "pathway to cancer."
"One great example is colon cancer, where Dr. White discovered the APC gene," says Prescott. "When the APC gene is damaged, you're on your pathway to colon cancer. But it's not enough just to know that the APC gene is damaged. What caused the damage? What happens after the damage?
"When you know there's the damaged APC gene, you can try to fix it. That's what most people typically try to do. But that hasn't worked well yet. That's trying to replace something that's been lost and there are very few drugs that can do that.
"So our thought was: let's try to see what happens after this gene is damaged," Prescott continues. "The loss of the function of that gene must cause other things to be increased, leading to abnormal growth. If we can find those next steps, that gives us a target.
"See, if something's increased, then if I can just block that increase, that may block the cancer. That's what traditional medications do: block an increase, not replace a decrease.
"An example is in my own laboratory. One of the things we work on is an enzyme called COX-2. An increase in COX-2 is absolutely required on the pathway between damage in an APC gene and the development of colon cancer. So we're trying to discover the link between the loss of the APC gene and the turning on of COX-2. If we can keep COX-2 turned off, maybe we can block the cancer."
The Plan of Attack
Standing in the way of finding cures is the way that cancer patients are treated. "The system for dealing with cancer patients is not ideal," Prescott says. "[Dr. Simone] calls it 'the handoff system.'"
Prescott says the handoffs start with the surgeon who operates. Once the surgery has been performed, the patient is "handed off" to the radiation therapist, who, in turn, hands the patient off to an oncologist, who hands the patient off to a pain management specialist.
"There's no plan," Prescott laments.
To tackle the handoff problem, HCI is creating the Huntsman Cancer Care Program (HCCP), which Simone directs.
"The program is a combination of patient care here [at the Institute's building], plus an outreach to oncologists in the region to participate in the exchanging of information about patients," Simone says. The joint clinical oncology program includes cancer specialists with Intermountain Health Care and the University of Utah. "We're trying to capture information on as many patients as possible to know where we are as far as finding the most effective treatment protocols."
 |
|
Postdoctoral
fellow Anjali Kalyani and
Assistant Professor David Jones |
With childhood cancers, most patients become part of clinical trials. This provides a plan for treatment, with follow-ups and frequent feedback. It also provides the opportunity to capture information vital to the understanding of all the variables found in cancer care, such as what treatment has worked best for which cancer at what stage and under what circumstances.
The cure of many childhood cancers has been attributed to this high participation in clinical trials.
"But only about two percent of adults with cancer go into clinical trials," Simone says. "So for 98 percent of the patients you have no systematic collection of information. It's very hard to make changes in practice patterns unless you know what actually happened." Which is why Utah families such as Lynn Trenbeath's, and clinical trials such as the study of Tamoxifen and Raloxifene for the prevention of breast cancer in high-risk women, are so essential to what HCI does.
Simone says that having as many clinical oncologists from the community as possible participate by using a software program that allows for the compilation of a large database and the exchange of information is the goal.
"We give all of the information coming in back to the doctors," Simone says. "Collectively [we'll] make decisions on whether the approach that we are using needs to be modified. We're really trying to foster a comprehensive plan."
The idea is to provide "one-stop shopping," with all the experts in one room to establish a plan for the patient's care. "The plan might change because things happen," says Simone, "but at least [the healthcare providers involved are] on the same page."
 |
| Dr. Frank Fitzpatrick |
As for the seemingly overwhelming complexity and number of cancers, the directors at HCI maintain that going back to the basics and applying the genetic understanding that has made the University a world leader will be the key.
"There are certain underlying principles that apply in all cancers," says Simone. "So a lot of the basic research is looking at those principles and hoping that they will impact a whole series of different cancers."
Bringing the Curtain Down on Cancer
"There are hundreds of new interventions and therapeutics out there," says White. "A few of them are sitting here in our laboratories. Most won't work, but some will. And it is those 'some' that will make the big difference. So if I had to make a prediction, I would say the next several decades are going to see, effectively, the end of cancer. Not this year, not the next year, and I can't say that it'll happen in seven-point-five years. But each of these [different kinds of cancer] will have its solution. It is not unreasonable to imagine new therapeutics which are going to greatly reduce early death and disease. That's the heart of the matter."
The optimism that even pragmatic scientists such as Prescott, White, and Simone share is embodied in the design of the building that is a visual symbol of their anti-cancer message. The glamorous, glass-fronted, six-story building rises to a sharp point, a design element that was incorporated to represent cutting-edge research, according to Jon Huntsman Jr. The stair tower on its northeast side is illuminated with fiber-optic light, which he calls a "beacon of hope that will be lit until the battles with cancer are won." And beneath the facade, in laboratory after laboratory, the unrelenting detective work takes place. That is the Huntsman Cancer Institute's generative core.
—Adam Olson BS'99 is a former writer for the Daily Utah Chronicle who writes for the Davis County Clipper and Utah Spirit Magazine.
Copyright 2000 by The University of Utah Alumni Association